How I Cracked the Code to Better Digestion — My Real Tracking Journey
Digestive issues affect millions, yet many suffer in silence, not knowing how to track or improve their gut health. I was one of them—until I started paying attention. By simply monitoring my body’s signals, food choices, and daily habits, I began to see patterns that transformed my comfort and energy levels. This is not a miracle cure, but a practical, science-backed approach to understanding your digestion like never before. What started as a personal experiment turned into a life-changing habit, revealing connections between what I ate, how I felt, and why certain days left me sluggish or bloated. The truth is, your digestive system speaks to you every day—you just need to learn how to listen.
The Hidden Struggle: Why Digestive Health Often Gets Ignored
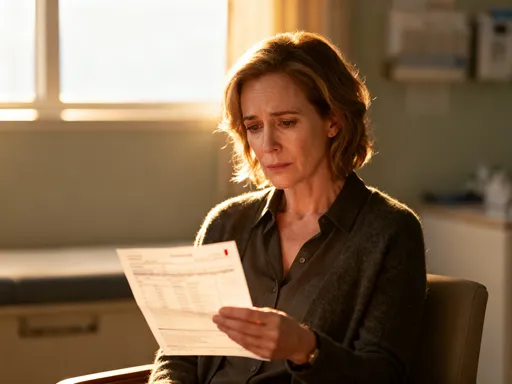
Digestive discomfort is more common than many realize, yet it remains one of the most under-discussed health concerns, especially among women over30. Bloating, gas, constipation, or irregular bowel movements are often brushed off as normal parts of life, especially during hormonal shifts or busy seasons. However, persistent symptoms are not something to simply endure. According to the American Gastroenterological Association, over60 million Americans experience gastrointestinal issues annually, with many cases going unreported due to embarrassment or the belief that nothing can be done. These symptoms can significantly impact daily functioning—reducing energy, affecting mood, and even disrupting sleep.
For years, I accepted bloating after meals and afternoon fatigue as inevitable. I blamed aging, stress, or lack of time for self-care. It wasn’t until I missed a family outing due to abdominal discomfort that I realized how much my digestion was controlling my life. I wasn’t alone. Many women in their30s,40s, and50s quietly manage these symptoms without seeking solutions, often because they don’t recognize them as signs of imbalance. The normalization of digestive distress prevents people from exploring root causes, whether dietary, lifestyle-related, or linked to chronic stress. But discomfort is not normal—it’s a signal.
Ignoring digestive signals can lead to a cycle of worsening symptoms and reduced quality of life. What begins as occasional bloating may evolve into consistent discomfort, food avoidance, or reliance on over-the-counter remedies. The gut plays a central role in overall health, influencing immunity, nutrient absorption, and even mental well-being. When digestion is compromised, the entire body feels the effect. Recognizing that these symptoms are not trivial—but rather valuable clues—is the first step toward meaningful change. The journey to better gut health begins not with a drastic diet or supplement, but with awareness.
Why Tracking Matters: Turning Guesswork into Real Clarity
Most people approach digestive issues with guesswork. They eliminate entire food groups based on trends, rely on anecdotal advice, or make random changes without knowing what truly affects them. This trial-and-error method often leads to frustration and confusion. What transformed my experience was shifting from guessing to observing. Tracking my daily habits and symptoms allowed me to move from assumptions to evidence. Science supports this approach: studies in behavioral medicine show that self-monitoring increases self-awareness and improves outcomes in managing chronic conditions, including irritable bowel syndrome (IBS) and functional digestive disorders.
When you track consistently, you begin to see patterns that are invisible in the moment. For example, I assumed my bloating was caused by eating too much at dinner. But after two weeks of logging, I discovered it wasn’t portion size—it was eating within three hours of bedtime. Another surprise: my worst energy crashes didn’t follow meals high in sugar, but days when I skipped breakfast entirely. Without data, I would have continued blaming the wrong things. Tracking turned vague discomfort into clear, actionable insights.
The power of tracking lies in its ability to personalize health. What triggers symptoms in one person may have no effect on another. General advice like “avoid gluten” or “eat more fiber” doesn’t account for individual differences. By collecting your own data, you create a customized roadmap. This method is not about perfection—it’s about progress. Each entry builds a clearer picture of how your body responds to food, stress, sleep, and movement. Over time, the accumulation of small observations leads to big revelations. And unlike quick-fix diets, this knowledge stays with you, empowering long-term choices.
What to Track: The Core Elements of Digestive Health Monitoring
To get meaningful results, it’s important to track the right factors. I developed what I call the “Digestive Health Dashboard,” a simple framework focusing on five key areas: food intake, bowel movements, energy levels, mood, and sleep. These elements are interconnected, and changes in one often affect the others. For instance, poor sleep can slow digestion, while certain foods may disrupt both mood and energy. By monitoring all five, you gain a holistic view of your gut-brain connection and overall well-being.
Food intake is the most obvious starting point. This doesn’t mean counting every calorie or weighing portions. Instead, note what you eat, the time of day, and how you felt during and after the meal. Did a morning smoothie leave you energized or bloated? Did a late-night snack cause restlessness? Paying attention to timing, combinations, and portion sizes reveals subtle but important patterns. Equally important is tracking bowel movements—frequency, consistency, and ease. While this may seem private or uncomfortable to record, it’s one of the most direct indicators of digestive function. Tools like the Bristol Stool Chart, used in clinical settings, can help standardize observations without judgment.
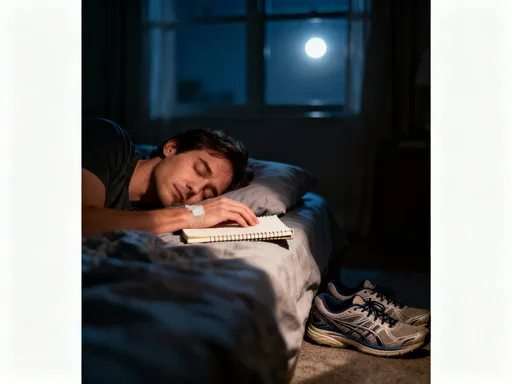
Energy levels and mood are often overlooked in digestive health, yet they are deeply linked. Many report feeling mentally foggy or irritable when digestion is off. I started rating my energy and mood on a scale of1 to5 each day, noting any shifts. Over time, I noticed that days with stable energy also had regular digestion and better sleep. Sleep quality, in turn, influenced my food cravings and stress levels the next day. Tracking these elements creates a feedback loop, showing how lifestyle choices ripple through the body. The goal is not to obsess over numbers, but to spot trends that guide better decisions.
How to Start: Building a No-Stress Tracking Routine
Starting a tracking habit can feel overwhelming, especially for busy women juggling work, family, and personal responsibilities. The key is simplicity. I began with just two entries per day—morning and evening—using a basic notebook. In the morning, I noted sleep quality and energy. At night, I recorded meals and bowel movements. This took less than three minutes. Over time, the routine became automatic, like brushing my teeth. The goal is not to create another chore, but to integrate tracking into existing habits.
Linking tracking to daily rituals increases consistency. I paired it with my evening tea, reviewing the day while unwinding. Others find success by journaling during breakfast or right before bed. The timing should fit naturally into your rhythm. Apps can help, but they’re not required. Some popular tools include MyFitnessPal for food logging, CareClinic for symptom tracking, and even voice notes for quick reflections. The best method is the one you’ll actually use. Paper journals, digital notes, or spreadsheets all work—choose what feels easiest and most sustainable.
Common pitfalls include overcomplicating the process, aiming for perfection, or losing motivation after a few days. To avoid this, start small. Focus on one or two factors at first. If you miss a day, don’t quit—just resume the next day. Progress, not perfection, is the goal. I found that after about10 days, tracking became second nature. Seeing early patterns—like improved energy on days I drank more water—provided motivation to continue. Over time, the habit transformed from a task into a form of self-care, a daily check-in with my body.
Decoding the Data: Spotting Patterns That Actually Help
After four weeks of consistent tracking, I reviewed my logs and began to see clear patterns. The most surprising discovery was my sensitivity to dairy. I had always considered myself “fine” with milk and cheese, but the data told a different story. On days I consumed dairy—especially in the evening—I experienced bloating, disrupted sleep, and lower energy the next morning. I hadn’t noticed this in real time, but seeing it laid out in writing made the connection undeniable. Another trigger was late-night eating. Even healthy meals after8 p.m. led to sluggish digestion and restlessness, regardless of content.
Interpreting the data requires attention to timing, frequency, and intensity. A single episode of bloating after a rich meal isn’t cause for concern. But if bloating occurs daily after eating certain foods, a pattern emerges. I used a simple rating system:1 for no symptoms,5 for severe discomfort. Over time, clusters of high ratings pointed to consistent triggers. This method helped distinguish between occasional indigestion and true sensitivities. It also revealed lifestyle factors—on high-stress days, even safe foods caused discomfort, suggesting stress was amplifying my gut response.
Differentiating between food sensitivities and lifestyle influences is crucial. Food sensitivities often produce predictable reactions—same food, same symptom, same timing. Lifestyle factors like stress, dehydration, or poor sleep tend to create generalized symptoms that vary day to day. For example, dehydration led to occasional constipation, while stress caused overall digestive slowdown. By tracking multiple factors, I could isolate variables and test changes one at a time. This eliminated confusion and built confidence in my conclusions. The data didn’t lie—and it gave me the clarity to act.
From Data to Action: Making Changes That Stick
Seeing the patterns was empowering, but real change came from acting on them. I started with small, manageable adjustments. First, I eliminated dairy for two weeks. I didn’t cut it out permanently—just long enough to reset and test. During that time, my bloating decreased significantly, and my energy stabilized. When I reintroduced dairy, I did so one product at a time—first yogurt, then cheese, then milk. This method, known as an elimination and reintroduction protocol, is supported by clinical nutrition guidelines for identifying food sensitivities. It allowed me to pinpoint exactly which products caused issues, rather than assuming all dairy was problematic.
Another change was adjusting meal timing. I shifted dinner earlier, aiming to finish eating at least three hours before bed. This simple change improved my sleep quality and reduced nighttime discomfort. I also began eating more slowly, chewing thoroughly, and avoiding distractions during meals. These mindful eating practices, recommended by digestive health experts, support optimal digestion by activating the parasympathetic nervous system. Over time, I noticed fewer instances of indigestion and greater satisfaction from meals, even with smaller portions.
Trial and error was essential. I tested one change at a time to see its isolated effect. For example, I focused only on hydration for a week, increasing water intake to half my body weight in ounces daily. The result? More regular bowel movements and less bloating. Once that change felt natural, I moved to the next. This step-by-step approach prevented overwhelm and built sustainable habits. I also shared my logs with a registered dietitian, who helped interpret the data and offered personalized guidance. Professional input was invaluable in confirming my observations and ensuring nutritional balance during dietary changes.
Beyond the Gut: The Ripple Effects of Better Digestion
The benefits of improved digestion extended far beyond my stomach. Within a few weeks, I noticed deeper sleep, clearer skin, and sharper mental focus. My afternoon energy crashes became rare, and I felt more emotionally balanced. These improvements weren’t coincidental. Research shows that a healthy gut microbiome influences sleep regulation, skin health, and cognitive function through the gut-brain-skin axis. By supporting my digestion, I was indirectly supporting multiple systems in my body.
Better digestion also improved my relationship with food. Instead of fear or confusion, I developed trust. I knew what my body responded to and could make informed choices without guilt or restriction. Social meals became enjoyable again, not sources of anxiety. I learned to adapt—bringing a safe dish to gatherings or choosing restaurants with flexible options. This sense of control reduced stress, which in turn supported further digestive healing. It was a positive feedback loop: better digestion led to less stress, which led to better digestion.
Perhaps the most profound shift was in how I viewed self-care. Tracking was no longer a chore but a daily act of listening to my body. It taught me patience, curiosity, and self-compassion. I stopped chasing quick fixes and started building lasting wellness. The journey reinforced a simple truth: small, consistent actions create meaningful change. Digestive health isn’t just about what you eat—it’s about how you live, how you rest, and how you pay attention. When you tune in, your body responds with clarity and resilience.
Tracking your digestive health isn’t about perfection—it’s about awareness. By tuning in to your body’s daily messages, you gain power over discomfort and build a foundation for lasting wellness. This journey isn’t quick, but it’s worth it. Your gut might just be the most honest messenger you’ve never truly listened to.