How I Tamed My Blood Sugar — A Real Talk on Staying Smart and Steady
Living with unpredictable blood sugar can feel like riding a rollercoaster without a seatbelt. I’ve been there—tired, foggy, and frustrated. It wasn’t until I shifted my mindset from quick fixes to a real system that things changed. This isn’t about magic pills or extreme diets. It’s about awareness, consistency, and small wins. If you’re ready to take control, not just react, this journey might just reframe how you see your health.
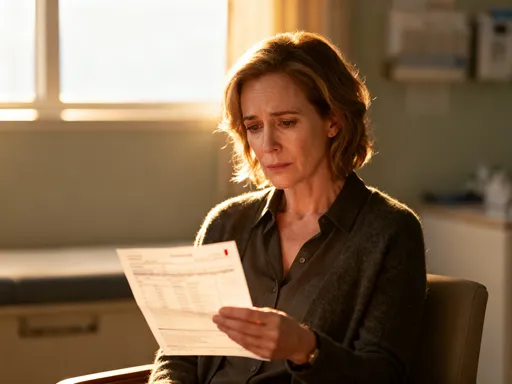
The Wake-Up Call: When Normal Felt Off
For years, I thought fatigue and mood swings were just part of being a busy woman juggling family, work, and home. Mornings started with coffee and a muffin, followed by a mid-morning crash that sent me reaching for candy. By 3 p.m., I was sluggish, irritable, and craving something sweet—again. I blamed stress, aging, or lack of sleep. But the truth was, my body was sending signals I wasn’t trained to read.
The turning point came during a routine check-up. My fasting glucose was higher than normal, and my doctor mentioned prediabetes—not a diagnosis, but a warning. I wasn’t overweight, didn’t eat fast food daily, and considered myself fairly active. How could I be at risk? That conversation shook me. It wasn’t about being unhealthy in the traditional sense; it was about imbalance. My energy swings, cravings, and mental fog weren’t quirks—they were symptoms of blood sugar fluctuations.
What I learned next changed everything: blood sugar issues don’t only affect people with diabetes. Millions of adults, especially women over 30, experience insulin resistance or glucose instability without a formal diagnosis. These silent shifts can increase the risk of type 2 diabetes, heart disease, and weight gain over time. Ignoring the early signs isn’t just risky—it’s common. But it doesn’t have to be inevitable. Recognizing the pattern was my first step toward real change.
Understanding Blood Sugar: What Most People Get Wrong
Blood sugar, or glucose, is the body’s primary fuel source. When we eat, especially carbohydrates, our digestive system breaks them down into glucose, which enters the bloodstream. In response, the pancreas releases insulin—a hormone that acts like a key, unlocking cells so glucose can enter and be used for energy. This process is natural and essential. But when it becomes imbalanced, problems arise.
One of the biggest misconceptions is that only people with diabetes need to care about blood sugar. In reality, even those with normal lab results can experience glucose spikes and crashes that affect how they feel day to day. These fluctuations can lead to fatigue, brain fog, irritability, and cravings—especially for sugary or starchy foods—which only worsen the cycle. Over time, repeated spikes can reduce the body’s sensitivity to insulin, a condition known as insulin resistance.
Another myth is that avoiding sugar alone is enough. While cutting back on added sugars is important, the quality and combination of all carbohydrates matter. White bread, pasta, and even some fruit juices can spike glucose just as quickly as candy. The key isn’t elimination—it’s balance. Pairing carbohydrates with protein, healthy fats, and fiber slows digestion and prevents sharp rises in blood sugar. This approach supports stable energy, reduces cravings, and helps maintain a healthy metabolism.
Understanding this system changed how I viewed food. It wasn’t about labeling foods as ‘good’ or ‘bad,’ but about how they worked together in my body. I began to see meals as tools for stability, not just satisfaction. This shift—from restriction to strategy—was empowering.
Building a System, Not a Shortcut
Early on, I tried quick fixes: juice cleanses, low-carb extremes, and skipping meals to ‘reset’ my system. Each brought temporary results, followed by rebound hunger and fatigue. I realized I wasn’t building habits—I was reacting. Sustainable health isn’t about dramatic changes that burn out in weeks. It’s about creating a system that fits into real life, one that supports your body consistently, not occasionally.
A successful system has several core components. First is routine. Going to bed, waking up, and eating meals at consistent times helps regulate the body’s internal clock, which influences insulin sensitivity. Irregular eating patterns can confuse the body’s metabolic signals, making it harder to manage glucose effectively. Establishing a daily rhythm—even on weekends—creates predictability that supports balance.
Second is food quality. This doesn’t mean perfection. It means choosing whole, minimally processed foods most of the time. Whole grains, vegetables, legumes, lean proteins, and healthy fats form the foundation. These foods provide steady energy and essential nutrients without causing sharp glucose spikes. Occasional treats are fine—what matters is the overall pattern.
Third is movement. Physical activity helps muscles use glucose more efficiently, even without weight loss. You don’t need hours at the gym. Short walks, stretching, or household chores all contribute. The goal is consistency, not intensity. Fourth is sleep. Poor or inconsistent sleep disrupts hormones that regulate hunger and insulin, making blood sugar control harder. Aiming for 7–8 hours of quality sleep supports metabolic health.
Finally, tracking. This doesn’t have to mean constant finger pricks or apps. Simple awareness—like noticing how you feel after meals—can be powerful. Over time, patterns emerge. You start to recognize which foods leave you energized and which cause a crash. This self-knowledge is the foundation of long-term control.
My Daily Routine: A Real-Life Blood Sugar Game Plan
Mornings set the tone for my day. I start with a large glass of water—hydration after a night’s sleep helps kickstart metabolism and supports circulation. I avoid coffee on an empty stomach, which can spike cortisol and affect glucose. Instead, I aim for a balanced breakfast within an hour of waking, combining protein, fiber, and smart carbohydrates.
One of my go-to meals is Greek yogurt with berries, chia seeds, and a sprinkle of nuts. The protein and fat slow digestion, while the fiber from berries and chia helps regulate glucose absorption. Another option is scrambled eggs with spinach and avocado on whole grain toast. These meals keep me full and focused, without the mid-morning slump. I avoid sugary cereals, pastries, or fruit juices—they may taste good, but the energy crash isn’t worth it.
Lunch is built around balance. I aim for half the plate to be non-starchy vegetables—like broccoli, salad greens, or roasted peppers. A quarter is lean protein—chicken, fish, tofu, or beans. The remaining quarter is a complex carbohydrate—quinoa, brown rice, or sweet potato. This plate method, recommended by many nutrition experts, naturally supports glucose stability without calorie counting.
Snacking is often where blood sugar goes off track. I used to grab granola bars or crackers, not realizing many are loaded with hidden sugars and refined carbs. Now, I choose snacks that combine protein and fiber. Examples include apple slices with almond butter, cottage cheese with cucumber, or a small handful of mixed nuts and a few grapes. These options satisfy hunger and prevent overeating at the next meal. I also pay attention to timing—eating every 3–4 hours helps maintain steady energy.
Dinner is lighter but still balanced. I focus on lean protein and vegetables, with a modest portion of whole grains if needed. I avoid large, carb-heavy meals late at night, as they can disrupt sleep and glucose levels. A sample dinner might be grilled salmon, roasted Brussels sprouts, and a small serving of wild rice. I eat slowly, without distractions, which helps with portion control and digestion.
Evening routines matter too. I avoid sugary desserts, but I don’t deny myself entirely. A square of dark chocolate or a small bowl of fruit with yogurt satisfies my sweet tooth without derailing progress. The key is mindfulness—enjoying it slowly, without guilt.
Movement That Works—Even on Busy Days
Exercise doesn’t have to be intense to help blood sugar. In fact, one of the most effective strategies is something most of us can do: walking. After meals, especially those containing carbohydrates, a 10–15 minute walk can significantly reduce glucose spikes. Muscle movement helps the body use glucose without relying solely on insulin. This is especially helpful after dinner, when activity levels naturally drop.
On busy days, I look for small opportunities to move. I’ll stretch while watching the news, take the stairs instead of the elevator, or do a few minutes of gentle yoga before bed. Even standing up and pacing during phone calls adds up. The goal isn’t to burn calories—it’s to keep the body active and responsive.
I also use a simple daily step goal—around 7,000 to 8,000 steps. I don’t track obsessively, but having a general target keeps me aware. On weekends, I enjoy longer walks with family or a bike ride in the park. These aren’t workouts in the traditional sense, but they support insulin sensitivity and overall well-being.
Strength training is another helpful tool. Building muscle increases the body’s capacity to store and use glucose. Two or three short sessions per week—using body weight, resistance bands, or light weights—can make a difference. I focus on form and consistency, not heavy lifting. Even 15 minutes at home can be effective.
The biggest lesson? Movement doesn’t have to be perfect. A short walk after lunch is better than nothing. Standing while folding laundry counts. The body thrives on regular activity, not marathon sessions. Over time, these small efforts create lasting benefits for blood sugar control and energy levels.
Mindset and Awareness: The Hidden Lever in Blood Sugar Control
One of the most overlooked factors in blood sugar management is the mind. Stress, lack of sleep, and emotional eating can all trigger glucose spikes—even if your diet is otherwise balanced. When we’re stressed, the body releases cortisol and adrenaline, hormones that signal the liver to release stored glucose. This is helpful in true emergencies, but when stress is constant, it keeps blood sugar elevated.
I’ve learned to recognize my triggers. For me, late-night work, family conflicts, or poor sleep often lead to cravings and poor food choices. Instead of reacting, I’ve built in small mindfulness practices. Five minutes of deep breathing, journaling before bed, or a short walk in nature help reset my nervous system. These aren’t quick fixes, but they build resilience over time.
Another powerful tool is tracking. I started with a simple food and mood journal. For two weeks, I wrote down what I ate, how I felt afterward, and my energy levels. Patterns quickly emerged. I noticed that white bread left me sluggish, while a protein-rich breakfast kept me focused. I didn’t need a continuous glucose monitor to see the effects—my body was telling me what worked.
Over time, this awareness became automatic. I began to eat more intuitively, tuning into hunger and fullness cues. I stopped eating out of boredom or emotion. This shift wasn’t about willpower—it was about education. The more I understood my body’s responses, the easier it became to make supportive choices without feeling deprived.
Mindset also means letting go of perfection. There will be days when plans fall apart—family events, travel, or unexpected stress. Instead of guilt, I practice self-compassion. One meal doesn’t define my health. What matters is returning to balance, not staying perfect. This gentle approach makes the journey sustainable.
Staying on Track Without Burning Out
Sustainability is the true measure of success. Any system that feels like punishment will eventually fail. I’ve learned to design a lifestyle that supports me, not one that exhausts me. This means allowing flexibility, celebrating small wins, and building support.
Slip-ups are normal. I’ve eaten cake at birthdays, had late-night snacks, or skipped walks during busy weeks. Instead of self-criticism, I ask myself: What can I learn from this? Was I tired? Stressed? Bored? Understanding the ‘why’ helps me adjust, not quit. Progress isn’t linear, and health is a lifelong journey, not a destination.
Support makes a difference. I’ve shared my goals with my family, who now join me in choosing balanced meals. My partner walks with me after dinner, and my kids enjoy helping with meal prep. I also use simple tools—like a habit tracker app or calendar reminders—to stay consistent. Regular check-ins with my doctor help me monitor progress and stay motivated.
It’s important to note that this system complements medical care—it doesn’t replace it. If you have prediabetes, diabetes, or other health conditions, working with a healthcare provider is essential. They can help interpret lab results, recommend appropriate testing, and guide treatment. My experience isn’t a prescription; it’s a personal example of how small, consistent changes can lead to meaningful results.
Blood sugar control isn’t just a medical goal—it’s a daily act of self-care. By building a personal system rooted in awareness and consistency, anyone can move from feeling reactive to feeling in charge. It’s not about perfection, but progress. And once you start seeing the ripple effects—more energy, better focus, improved mood—you’ll realize it’s not just about health. It’s about living better, one steady day at a time.