Strong Bones for Life: My Long-Term Journey to Better Skeletal Health
You might not think about your bones every day, but they’re the quiet foundation of everything you do. I didn’t either—until small aches became harder to ignore. Over time, I realized bone health isn’t about quick fixes, but consistent, smart choices. This is how I took control, not just to prevent problems, but to build lasting strength from the inside out. Bone health is often invisible until it’s compromised, yet it shapes how we move, carry ourselves, and live independently as we age. What I’ve learned is that protecting your skeleton is not reserved for the elderly or those with diagnosed conditions—it’s a lifelong responsibility that begins long before symptoms appear.
The Silent Crisis: Why Bone Health Matters More Than You Think
Bone health operates in silence. Unlike a sore muscle or a racing heart, bones rarely send urgent signals until something goes wrong. Yet, beneath the surface, they are alive—constantly breaking down and rebuilding in a process known as remodeling. This natural cycle keeps our skeleton strong and adaptable. However, around age 30, the balance shifts. The rate at which bone tissue is lost begins to exceed the rate at which it’s replaced. For many, this change happens gradually, without noticeable symptoms, making it easy to overlook until a minor stumble results in a fracture that should never have occurred.
Bone mineral density—the measure of how much calcium and other minerals are packed into a segment of bone—is a key indicator of skeletal strength. Low bone density increases the risk of osteopenia and, eventually, osteoporosis, a condition where bones become porous and fragile. According to the International Osteoporosis Foundation, one in three women and one in five men over the age of 50 will experience an osteoporotic fracture. These are not just statistics—they represent real-life consequences: loss of mobility, chronic pain, and reduced independence.
Despite these risks, misconceptions persist. Some believe bone health is only a concern for older women. While postmenopausal women face higher risks due to declining estrogen levels, men also lose bone mass with age. Others assume that as long as they drink milk, their bones are protected. In reality, bone strength depends on a combination of factors far beyond calcium alone. The truth is, skeletal health is not a single issue but a complex interplay of nutrition, physical activity, hormones, and lifestyle habits that must be managed over decades.
Ignoring bone health until a diagnosis comes is like waiting for a bridge to crack before inspecting its structure. By then, repair is more difficult and less effective. The good news is that bone loss is not inevitable. With informed, consistent actions, it’s possible to slow, halt, or even reverse early declines. The key is starting early and viewing bone health not as a reaction to aging but as a proactive investment in long-term well-being.
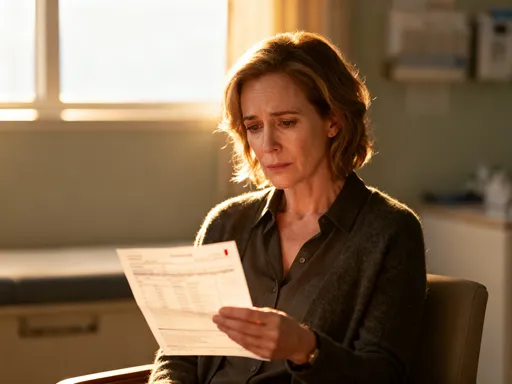
My Wake-Up Call: When Daily Aches Spoke Louder
My journey began not with a dramatic injury, but with a series of small, persistent discomforts. For months, I noticed a dull ache in my lower back after standing for long periods. I brushed it off as fatigue or poor posture. Then, a minor fall on a wet kitchen floor—a slip that should have been harmless—left me with a strained rib and a recovery that took weeks longer than expected. That was the moment I paused and asked myself: Why was my body responding so slowly to minor stress?
I wasn’t elderly. I was in my early 50s, active in daily life, and generally healthy. Yet, I realized I had stopped thinking about my body as something that needed ongoing maintenance. I ate fairly well, walked regularly, and avoided smoking and excessive alcohol. But I hadn’t given much thought to whether my habits were truly supporting my bones. The lingering discomfort and slow healing were signs I could no longer ignore. They weren’t emergencies, but they were signals—quiet warnings that my skeletal system might not be as resilient as I assumed.
What struck me most was the sense of losing physical confidence. I began hesitating before lifting grocery bags, stepping off curbs, or playing with my grandchildren. I didn’t want to live in fear of breaking a bone, but I also didn’t want to pretend everything was fine. This internal shift—from dismissal to awareness—was the turning point. I decided to take action not because I had a diagnosis, but because I wanted to prevent one. I wanted to feel strong, stable, and capable for years to come.
I started by consulting my healthcare provider, who recommended a bone density scan. The results showed early signs of bone loss—nothing severe, but enough to confirm that changes were underway. Rather than viewing this as a setback, I saw it as valuable information. It gave me clarity and motivation. I wasn’t broken; I was informed. And with that knowledge, I could make choices that supported long-term skeletal strength rather than waiting for a crisis to force my hand.
What Actually Builds Stronger Bones? Separating Hype from Science
When I began researching how to improve bone health, I was overwhelmed by conflicting advice. One source claimed that calcium supplements alone could prevent fractures. Another promoted exotic superfoods or high-dose vitamin regimens. I quickly realized that much of what’s marketed as “bone support” is based more on profit than proof. What I needed was not a miracle solution, but reliable, science-backed strategies that could be sustained over time.
The foundation of strong bones lies in three key areas: mechanical stress, nutrition, and hormonal balance. Unlike static structures, bones are dynamic tissues that respond to use. When subjected to force—such as weight-bearing activity—bone cells called osteoblasts are activated to deposit new mineralized tissue. This process, known as Wolff’s Law, explains why bones adapt to the demands placed on them. Just as muscles grow stronger with resistance, bones become denser when challenged. This means that movement isn’t just beneficial—it’s essential.
Nutrition plays a parallel role. Calcium is the most abundant mineral in bone, but it doesn’t work alone. It requires vitamin D to be absorbed in the intestines and directed into the skeleton. Without adequate vitamin D, the body cannot utilize calcium efficiently, regardless of intake. Magnesium, vitamin K2, and protein also contribute to bone matrix formation and mineralization. For example, vitamin K2 helps bind calcium to the bone structure, reducing the risk of calcium buildup in arteries—a critical balance often overlooked.
Yet, food is superior to supplements when possible. Studies, including those published in the Journal of Bone and Mineral Research, suggest that nutrients consumed through whole foods are more effectively absorbed and utilized than isolated forms in pills. This doesn’t mean supplements have no place—especially for individuals with documented deficiencies—but they should complement, not replace, a nutrient-rich diet. The goal is not perfection, but consistency: daily choices that collectively support skeletal renewal.
Hormonal health is another crucial, yet often invisible, factor. In women, estrogen plays a protective role in maintaining bone density. The sharp decline during menopause accelerates bone loss, which is why early intervention is so important. In men, testosterone levels influence bone strength, and low levels can contribute to fragility. While hormones are not something most people can directly control, lifestyle choices—such as maintaining a healthy weight, managing stress, and avoiding excessive alcohol—can support hormonal balance and, by extension, bone health.
Movement That Works: The Exercise Plan I Stick With
One of the most empowering realizations in my journey was understanding that I didn’t need a gym membership, expensive equipment, or extreme workouts to support my bones. What mattered most was consistency and the right type of movement. I focused on three categories of exercise: weight-bearing activities, resistance training, and balance work—all proven to enhance bone density and reduce fracture risk.
Weight-bearing exercises are those where your bones and muscles work against gravity. Walking became my cornerstone. I started with 20 minutes a day and gradually increased to 45 minutes, most days of the week. I made it enjoyable by walking in parks, listening to audiobooks, or meeting a friend. The rhythmic impact of each step sends gentle signals to the bones in my legs and spine, stimulating remodeling. Over time, I added short bursts of brisk walking to increase intensity without strain.
Resistance training followed. I began with bodyweight exercises—wall push-ups, seated leg lifts, and modified squats using a chair for support. These built strength safely and improved coordination. As I gained confidence, I incorporated light dumbbells and resistance bands. I focused on major muscle groups: legs, back, chest, and arms. Each session lasted 20 to 30 minutes, two to three times per week. The key was gradual progression—never pushing to pain, but always challenging myself slightly more than the week before.
Balance exercises were another essential component. Poor balance increases fall risk, which is especially dangerous when bones are fragile. I practiced simple routines: standing on one foot while brushing my teeth, heel-to-toe walking in the hallway, and gentle tai chi movements from online videos. These small habits improved my stability and coordination, giving me greater confidence in daily movements.
What made this plan sustainable was its flexibility. I didn’t aim for perfection. If I missed a day, I resumed without guilt. If I felt tired, I shortened the session. The goal was long-term adherence, not short-term intensity. Over months, I noticed real changes: less back stiffness, more energy, and a renewed sense of physical capability. Exercise stopped being a chore and became a form of self-care—a daily promise to honor my body’s need for movement.
Fueling Your Frame: Simple Dietary Tweaks That Make a Difference
Nutrition was another pillar of my approach, but I refused to adopt a rigid or restrictive diet. Instead, I focused on gradual, realistic changes that fit my lifestyle. I asked myself: How could I get more bone-supporting nutrients without overhauling my kitchen or sacrificing enjoyment?
I started by increasing my intake of calcium-rich foods. Dairy products like yogurt and cheese were already part of my routine, but I expanded to include non-dairy sources: fortified plant milks, tofu made with calcium sulfate, canned sardines with bones, and dark leafy greens like kale and bok choy. I learned that spinach, while nutritious, contains oxalates that reduce calcium absorption, so I prioritized low-oxalate greens. I didn’t aim for a specific number of milligrams each day, but I made sure calcium-rich foods appeared in at least two meals.
Vitamin D was trickier, since few foods contain it naturally. Fatty fish like salmon and mackerel helped, but I also relied on fortified foods—certain cereals, orange juice, and plant-based milks. However, the most reliable source was sunlight. I began spending 10 to 15 minutes outside most days, exposing my arms and face without sunscreen. This modest exposure, especially in the morning or midday, supported natural vitamin D synthesis. In winter months, when sunlight was limited, I discussed supplementation with my doctor and took a moderate dose based on blood test results.
Protein was another focus. While often associated with muscle, protein is also a key component of the bone matrix. I ensured each meal included a source—eggs, beans, lentils, poultry, or fish. I avoided extremely low-protein diets, which some older adults adopt due to digestive concerns, as they can weaken both muscle and bone.
I also paid attention to habits that could undermine my efforts. Excessive salt increases calcium excretion through urine, so I reduced processed foods and used herbs and spices for flavor. High caffeine intake—more than three cups of coffee a day—has been linked to reduced calcium absorption, so I limited myself to one or two cups. Alcohol, when consumed in excess, interferes with bone formation and increases fall risk, so I kept my intake within moderate guidelines: no more than one drink per day.
These changes weren’t about perfection. I still enjoyed occasional treats and dining out. The difference was awareness. I learned to make better choices most of the time, knowing that consistency—not occasional extremes—was what truly supported my bones.
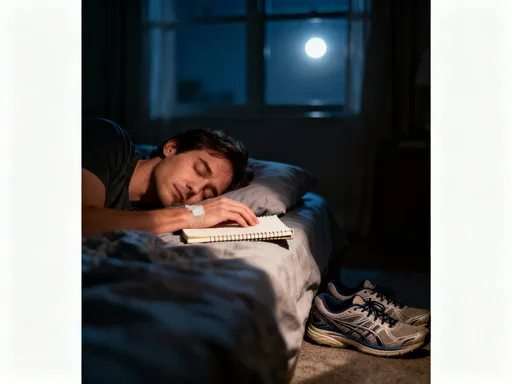
Lifestyle Levers: Sleep, Stress, and Daily Habits You Can’t Ignore
As I deepened my understanding of bone health, I realized it wasn’t just about food and exercise. Other lifestyle factors played a quiet but powerful role. Sleep, stress management, and daily routines all influenced the biological environment in which bones rebuild.
Sleep, for instance, is when much of the body’s repair occurs. Growth hormone, which supports tissue regeneration, is primarily released during deep sleep. Chronic sleep deprivation disrupts this process and increases inflammation—both of which can impair bone remodeling. I examined my own habits and realized I often stayed up late watching television or scrolling on my phone. I began setting a consistent bedtime, creating a calming evening routine: dimming lights, drinking herbal tea, and reading a book. Over time, my sleep quality improved, and I noticed a difference in my overall energy and recovery.
Chronic stress was another hidden factor. When the body is under constant stress, it produces elevated levels of cortisol, a hormone that, in excess, can accelerate bone breakdown and suppress bone formation. While some stress is unavoidable, I realized I wasn’t managing it effectively. I started incorporating mindfulness practices—five minutes of deep breathing each morning, short walks in nature, and journaling when I felt overwhelmed. These small acts didn’t eliminate stress, but they helped me respond to it more calmly, reducing its long-term toll on my body.
I also reevaluated habits like smoking and alcohol use. I had never been a smoker, but I knew it was one of the most damaging behaviors for bone health, reducing blood supply to bones and impairing calcium absorption. For those who do smoke, quitting remains one of the most impactful steps they can take. Alcohol, as mentioned earlier, affects bone metabolism and balance. By keeping consumption moderate, I protected both my skeletal system and my overall well-being.
These lifestyle adjustments didn’t require dramatic overhauls. They were small, sustainable shifts—like going to bed 30 minutes earlier or choosing water over soda—that collectively created a healthier internal environment for bone renewal.
Staying on Track: How I Stay Consistent Without Burnout
The biggest challenge wasn’t starting—it was staying consistent. Like many, I’ve experienced the cycle of enthusiasm followed by burnout. What helped me maintain momentum was shifting my mindset from short-term fixes to lifelong habits. I stopped chasing immediate results and focused instead on showing up, even in small ways.
I set non-scale goals—outcomes that weren’t measured by numbers but by how I felt. Could I climb a flight of stairs without catching my breath? Could I carry my suitcase without back pain? These were tangible signs of progress that kept me motivated. I also kept a simple journal, not to track every meal or minute of exercise, but to note how I felt each week. On days when I lacked energy, I reminded myself that rest was part of the process, not a failure.
I built accountability gently. I shared my goals with a close friend who also cared about health, and we checked in weekly. We didn’t compete—we encouraged. Sometimes, just knowing someone else was on a similar path made a difference. I also scheduled movement into my calendar, treating it like any other important appointment. This simple act increased follow-through and reduced the chance of skipping due to busyness.
Most importantly, I embraced imperfection. There were weeks when I traveled and my routine lapsed. There were days when I ate more sweets than planned. Instead of quitting, I practiced self-compassion. I reminded myself that bone health is a long game. Missing a workout or eating a less nutritious meal didn’t erase months of progress. What mattered was the overall pattern—the cumulative effect of most days being supportive.
Building More Than Stronger Bones
Looking back, I see that my journey was never just about bones. It was about reclaiming a sense of agency over my health and future. Strong bones mean more than avoiding fractures—they mean maintaining independence, enjoying time with loved ones, and moving through life with confidence and ease.
The habits I’ve adopted—daily walks, mindful eating, better sleep—have improved more than my skeletal system. They’ve enhanced my energy, mood, and overall resilience. I’ve learned that health is not a destination but a continuous practice, built one small choice at a time.
Bone health is not about fear. It’s about empowerment. It’s about understanding that your body is responsive, adaptable, and capable of renewal at any age. You don’t need to be perfect. You just need to be consistent. Every walk, every nutritious meal, every night of restorative sleep is a deposit into your body’s long-term strength.
If you’re noticing small aches, feeling less resilient, or simply want to prepare for the years ahead, know that it’s never too early or too late to start. Talk to your healthcare provider, get informed, and take one step at a time. Because taking care of your skeleton isn’t a burden—it’s a quiet, powerful act of self-respect. It’s an investment in a future where you can stand tall, move freely, and live fully. Always consult a healthcare provider before making significant health changes.