What Aging Quietly Hides: How Early Clues Can Change Your Health Story
We all age, but not all aging looks the same. Behind the surface, subtle shifts in energy, sleep, or skin might signal deeper health changes long before symptoms appear. I’ve learned this the hard way—what seemed like normal fatigue turned out to be an early warning. Catching these signs early isn’t about fear; it’s about power. It’s the difference between reacting and preventing. This is why understanding your body’s quiet signals isn’t just smart—it’s life-changing. The choices we make today, often in silence and routine, shape the quality of our years ahead. Recognizing the earliest hints of imbalance allows us to act with intention, not urgency.
The Silent Shift: When Aging Begins Before You Notice
Aging is often measured in birthdays, but the real story unfolds beneath the surface. Chronological age—the number of years since birth—is only part of the picture. Biological age, determined by the functional state of cells, tissues, and systems, can differ significantly and is a more accurate predictor of health outcomes. Research shows that internal aging processes, such as cellular senescence, mitochondrial decline, and chronic low-grade inflammation, can begin decades before visible signs like wrinkles or graying hair appear. These changes are not sudden; they accumulate silently, often without immediate discomfort or diagnosis.
Many women in their 30s and 40s report feeling generally fine, yet experience unexplained shifts—slightly less stamina, longer recovery after physical effort, or occasional mental fog. These are not simply quirks of busy lives. They may reflect early metabolic changes, hormonal fluctuations, or immune system adjustments. For example, insulin sensitivity can decline gradually, setting the stage for metabolic syndrome long before blood sugar levels cross diagnostic thresholds. Similarly, joint stiffness after sitting may hint at early cartilage wear or inflammatory activity, not just aging.
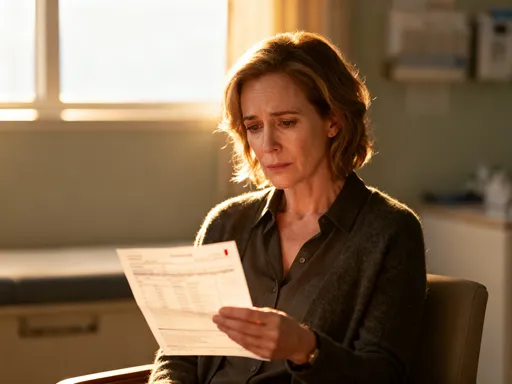
The misconception that “no symptoms mean no problems” is one of the most dangerous assumptions in health. Diseases such as hypertension, osteoporosis, and even certain cancers can develop over years without obvious signs. By the time symptoms emerge, the condition may be more advanced and harder to reverse. This delayed recognition is especially common in women, who often prioritize family and work over personal health checks. The reality is that the body communicates early—through fatigue, disrupted sleep, or minor aches—but these signals are easily dismissed as stress or normal aging.
Understanding this silent shift reframes how we view health. It is not a static state but a dynamic process influenced daily by lifestyle, environment, and genetics. The goal is not to stop aging, which is natural and inevitable, but to slow the rate of biological aging and extend healthspan—the years lived in good health. Recognizing that internal changes precede outward signs empowers individuals to act before decline becomes irreversible. This awareness is the first step toward a more intentional, informed approach to long-term well-being.
Why Early Detection Matters More Than We Think
Chronic diseases such as type 2 diabetes, heart disease, and certain cancers do not appear overnight. Scientific evidence shows that the biological processes leading to these conditions often begin five to ten years before clinical diagnosis. For instance, insulin resistance can develop silently, with blood glucose levels remaining within the “normal” range while metabolic stress builds. Similarly, atherosclerosis—the buildup of plaque in arteries—can progress for years without symptoms, only to result in a sudden cardiovascular event. These long development periods offer a critical window for intervention, yet they are frequently missed due to lack of awareness or routine screening.
Early detection transforms the trajectory of health. When conditions are identified in their initial stages, interventions are more effective, less invasive, and often reversible. A study published in The Lancet found that lifestyle changes implemented during pre-diabetes reduced the risk of progressing to full diabetes by up to 58%. Another study demonstrated that early blood pressure management significantly lowered the risk of stroke and heart failure over time. These findings highlight a fundamental truth: preventing disease is far more effective than treating it after it takes hold.
The benefits of early action extend beyond medical outcomes. They reduce the emotional and financial burden on families, minimize the need for long-term medications, and preserve independence and quality of life. When a woman in her 40s addresses rising cholesterol through diet and activity, she is not just lowering a number—she is protecting her future mobility, cognitive function, and vitality. Early intervention allows for gradual, sustainable changes rather than emergency measures later in life.
Moreover, early detection supports a shift from a reactive to a preventive healthcare model. Instead of waiting for a crisis, individuals can partner with healthcare providers to monitor trends, assess risks, and implement personalized strategies. This proactive approach aligns with the growing understanding that health is not the absence of disease but the presence of resilience. By focusing on early clues, women can take control of their health journey, making informed choices that compound over time. The power lies not in fear, but in foresight.
Your Body’s Whisper: Common Early Warning Signs You Might Ignore
The body communicates constantly, but its messages are often subtle—more whisper than alarm. Persistent low energy, even after adequate sleep, is one of the most common yet overlooked signs. While fatigue can stem from stress or busy schedules, it may also reflect underlying issues such as thyroid imbalances, iron deficiency, or poor blood sugar regulation. When energy dips become routine rather than occasional, they signal that something deeper may be at play. Ignoring these patterns can allow small imbalances to grow into larger health challenges.
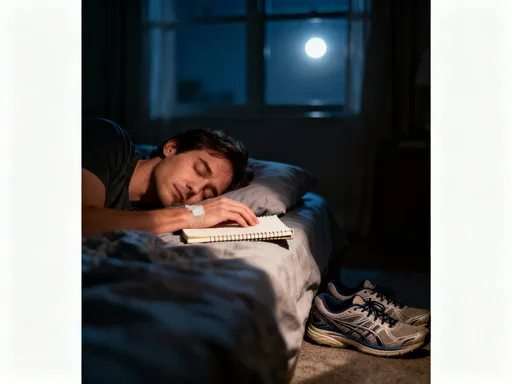
Sleep disturbances are another frequent clue. Difficulty falling asleep, frequent nighttime awakenings, or unrefreshing sleep may point to hormonal shifts, particularly during perimenopause, or to stress-related cortisol imbalances. Poor sleep quality is not just a nuisance; it is linked to increased inflammation, impaired immune function, and higher risk of metabolic disorders. Yet many women accept disrupted sleep as a normal part of aging, failing to recognize it as a modifiable factor that can be improved with targeted strategies.
Joint stiffness, especially in the morning or after inactivity, is often dismissed as “just getting older.” However, consistent stiffness may indicate early cartilage wear, low-grade inflammation, or vitamin D deficiency. Similarly, changes in skin texture—dryness, thinning, or slower wound healing—can reflect declining collagen production, hormonal changes, or nutritional gaps. These external signs are not merely cosmetic; they are visible markers of internal aging processes.
Other subtle signals include minor memory lapses, digestive changes, or shifts in mood and focus. Forgetting appointments, experiencing bloating without clear cause, or feeling more irritable than usual may seem minor, but when tracked over time, they can reveal patterns worth investigating. The key is consistency: isolated incidents are usually not concerning, but recurring or worsening symptoms deserve attention. These whispers are not meant to cause anxiety but to prompt curiosity and care. By learning to listen, women can respond with informed action rather than wait for louder, more urgent warnings.
Beyond the Mirror: Tools and Tests That Reveal Hidden Changes
While self-awareness is essential, objective tools can provide deeper insight into what’s happening beneath the surface. Routine blood tests are among the most accessible and valuable resources. Standard panels measure glucose, cholesterol, and liver function, but more comprehensive assessments can evaluate markers of inflammation such as C-reactive protein (CRP), insulin levels, and vitamin D status. These biomarkers offer a snapshot of metabolic and immune health, helping to identify imbalances before they become clinical conditions.
Body composition analysis goes beyond the scale by measuring muscle mass, body fat percentage, and visceral fat—the dangerous fat stored around organs. This information is particularly useful because two people with the same weight can have vastly different health risks based on fat distribution. Tools like bioelectrical impedance scales or DEXA scans provide detailed data that can guide nutrition and exercise choices. For example, declining muscle mass, a natural part of aging, can be slowed with strength training, but only if it is first recognized.
Wearable technology has made health tracking more convenient than ever. Devices that monitor heart rate variability (HRV), sleep stages, and activity levels offer real-time feedback on the body’s response to stress, recovery, and lifestyle habits. HRV, in particular, is a strong indicator of autonomic nervous system balance—low variability often reflects chronic stress or poor resilience. While these tools are not diagnostic, they help users identify patterns and make informed adjustments.
Emerging technologies like epigenetic clocks analyze DNA methylation patterns to estimate biological age. Though not yet routine in clinical practice, these tests are becoming more available through specialized labs and can reveal whether a person is aging faster or slower than their chronological age. Such insights can be powerful motivators for lifestyle change. However, it is important to remember that no test replaces a healthcare provider’s evaluation. These tools are most effective when used in conjunction with professional guidance, forming a partnership between personal awareness and medical expertise.
The Prevention Mindset: Shifting from Reactive to Proactive Health
True health begins with a mindset shift—from viewing wellness as the absence of illness to seeing it as an active, ongoing practice. This preventive mindset recognizes that daily choices shape long-term outcomes. It moves away from crisis management and embraces consistent, small actions that build resilience over time. For women managing households, careers, and relationships, this shift can feel challenging, but it is precisely this stage of life where prevention matters most.
The concept of healthspan—how many years one lives in good health—is gaining recognition as a more meaningful goal than lifespan alone. Living to 90 is valuable, but living to 90 with energy, mobility, and mental clarity is the real aim. Extending healthspan requires attention to foundational habits: quality sleep, balanced nutrition, regular movement, and stress management. These are not one-time fixes but lifelong practices that compound in benefit.
Sleep hygiene, for example, involves consistent bedtimes, limiting screen exposure before bed, and creating a restful environment. These simple steps improve sleep quality, which in turn supports hormone balance, immune function, and cognitive health. Similarly, managing stress through mindfulness, deep breathing, or time in nature helps regulate cortisol levels, reducing the long-term wear and tear on the body.
Movement is another cornerstone. It does not require intense workouts; regular walking, strength training, and flexibility exercises maintain muscle mass, support joint health, and improve circulation. The key is consistency, not intensity. When these habits are viewed not as chores but as acts of self-care, they become sustainable. The preventive mindset turns health into a daily practice of listening, responding, and nurturing—one that empowers women to take charge of their well-being with confidence and clarity.
Action Steps: What You Can Do Today to Stay Ahead
Knowledge is powerful, but action brings change. The first step is scheduling an annual check-up that includes meaningful biomarkers, not just basic tests. Discuss with your doctor the value of checking inflammation markers, hormone levels, and metabolic health, especially if there is a family history of chronic conditions. Be proactive in asking questions and requesting tests that provide insight into long-term risks.
Start a simple health journal to track daily patterns. Note energy levels, sleep quality, digestion, mood, and any physical symptoms. Over time, this record can reveal trends that might otherwise go unnoticed. For example, consistently low energy on certain days might correlate with diet or stress levels, offering clues for improvement. This practice fosters body awareness and provides valuable information to share with healthcare providers.
Incorporate wearable devices or apps to monitor activity, heart rate, and sleep. Use this data not for perfection, but for awareness. If sleep scores are consistently low, experiment with earlier bedtimes or reducing caffeine. If stress levels are high, try adding short walks or breathing exercises. Small, consistent adjustments are more effective and sustainable than drastic overhauls.
Finally, prioritize strength training and balanced nutrition. Include adequate protein to support muscle health, fiber for digestion, and healthy fats for brain and hormone function. Hydration and regular meals help stabilize energy and mood. These habits do not require drastic diets or expensive supplements—just thoughtful, consistent choices. The goal is progress, not perfection. By taking these steps today, women can build a foundation of resilience that supports vitality for years to come.
The Bigger Picture: Long-Term Health as a Daily Practice
Preventing chronic disease and supporting healthy aging is not about a single test, diet, or workout. It is a lifelong commitment expressed through daily choices. Each decision—to rest when tired, to eat nourishing food, to move the body, to seek answers—adds up over time. The benefits of early awareness and consistent action multiply with each passing year, leading to greater independence, vitality, and peace of mind in later life.
Viewing health as a quiet, consistent commitment changes the relationship with aging. It is no longer something to fear or resist, but a process to navigate with wisdom and care. Women who adopt this mindset often find that taking time for themselves is not selfish—it is essential. By honoring the body’s signals and responding with intention, they create a legacy of well-being for themselves and their families.
The journey of health is personal, but it does not have to be solitary. Support from healthcare providers, trusted resources, and community can make a meaningful difference. The most powerful tool, however, is awareness—the ability to hear the body’s whispers before they become shouts. With that awareness comes the power to change the health story, not through fear, but through informed, compassionate action. In the end, the goal is not just to live longer, but to live well—fully, vibrantly, and with purpose.